Allergy



Sleep apnea, snoring, insomnia, restless leg, effects of poor sleep on your health, and much more.





Asthma is characterized by inflammation and narrowing of airway a passage that is recurrent and reversible. This narrowing causes wheezing, shortness of breath, cough and a tight feeling in the chest. Secretion of mucus into the airway and swelling of the airway lining also occurs during an asthma attack, along with constriction of the smooth muscles surrounding the airways. All this pathology conspires to make it increasingly difficult to breath. Approximately 4,000 to 5,000 individuals in the U.S. die annually from asthma.
Asthma is very common. The CDC says that 8.3% of children and 7.0% of adults in the U.S. have asthma. It frequently occurs in individuals with hay fever, eczema or a family history of allergy. In most cases, normal growth and development occur. The lungs are not usually permanently damaged if asthma is properly cared for.
If you’re looking for a doctor who specializes in asthma treatments and lung infections in Midlands, Texas, feel free to get in touch with Dr. John D. Bray.
Common causes of asthma include allergens, viral infections, and environmental changes in humidity, temperature and barometric pressure. Environmental irritants such as cigarette smoke, air pollution, dust and chemical odors, exercise and emotional upsets can help set off asthma.

Other causes of wheezing and coughing are ruled out by the history, physical examination, pulmonary function tests, and chest x-ray. As in all things medical, the doctor spending time to take a good history at the start is absolutely primary. Pulmonary function tests are performed because they reflect how involved and sensitive the airways are. They determine if narrowing and obstruction of the breathing tubes is present.
Pulmonary function test are also used to monitor a patient is response to treatment. Even though medications may seem to have the symptoms of asthma under control, a pulmonary function test (PFT) can more accurately show any residual abnormality; therefore they are an invaluable tool in threating asthma. A pulmonary function test is to asthma as a blood pressure determination is to hypertension.
Dr. Bray will take a detailed, careful, comprehensive history from you about your respiratory, allergy and general health. If indicated by your history and physical examination allergy skin testing will be done to determine which allergens are likely to be playing a role in your asthma. A lung function test is always done. A chest x-ray is also usually obtained. These test are basic and very helpful in any these asthma work up.

Symptoms of an asthma attack are coughing, wheezing, and shortness of breath with a tight heavy feeling in the chest and difficulty breathing. When this occurs, the individual should:
If these measures don’t work or your asthma has flared up quickly it is time to see you physician promptly or go to the E.R.
The goal of asthma treatment is to control the asthma symptoms and normalize lung function. The individual should avoid substances or situations which can precipitate an attack. Knowing one's own pattern is extremely important in developing a medical program to that will keep you well. This can be the key to successful control. This is another reason why Dr. Bray takes time to get a thorough, careful history from each of his patients.
For the problems of exercise-induced asthma, medication needs to be taken prior to exercise; Physical fitness is encouraged for all asthmatics. The key to making exercise not intolerable but enjoyable is to take you basic medicine daily and premeditated in an expert manner before exercise. Almost all fairly young asthmatics who do not have other serious medical problems with good care, can enjoy sports, exercise, and even run hard and long without their asthma flaring.
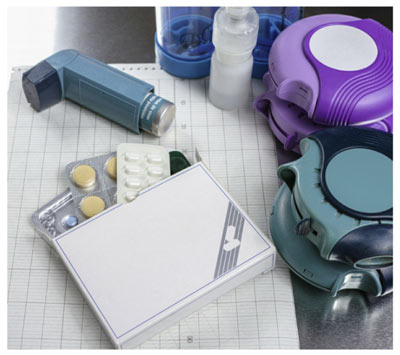
Several types of medication are used for asthma treatment. They are taken orally by inhalation or by injection. The right dosage, combination and type of medication must be determined for each individual patient.
Primary asthma medication available in inhaled form includes:
There are three basic types of devices used to deliver inhaled medications for asthma treatment The most common is the metered dose inhaler (MDI), which uses a chemical propellant to push the medication out of the inhaler, Chlorofluorocarbon (CFCs) used to be used in many MDls but have been replaced by other propellants. Nebulizers, deliver a fine liquid mists of medication through a tube or a "mask" that fits over the nose and mouth or is inhaled through the mouth using air or oxygen under pressure to power the nebulizer that turns the liquid medicine into a fine mist that can be inhaled. Rotary inhalers and other dry powder inhalers deliver medication without using chemical propellants.
Regardless of the type of inhalation device, effective delivery of medication to the lower airways is critical for the medication to work. For all such devices, education and training of patients and family by professional caregivers in the proper and effective use of these devices is an essential component of inhalation therapy. It is so important, in fact, that proper inhalation technique should be constantly asked about on visits with re-education and re-training as necessary. If you are unsure about using your inhalation device properly, ask for more training. Do not hesitate to do this.
Coordination of inhalation from inhalation devices varies from extremely easy with some devices (for example, nebulizers) to extremely difficult for some patients (for example, MDIs). A poor response to therapy can be due simply to such poor coordination between the device an a proper inhalation that little or no drug reaches the lower airways. A device called a spacer can improve delivery of inhaled medication from MDIs, making the problem difficult and more effective.
Spacers help deliver a greater amount of medication directly into the lower airways, where it is intended to go, rather than into the mouth throat. Many spacers fit on the end of an asthma inhaler. Some devices come with built-in spacers. Many people with asthma, especially young children, may have difficulties coordinating inhalation with using a metered dose inhaler. For these patients the use of a spacer is strongly recommended.
MDIs from which the drug is dispensed automatically when the patient breathes in from the inhaler are also available. The technique for inhalation from dry powder inhalers is different and may feel more "natural" than with MDIs to some patients. Spacers are not needed for dry powder devices.
Nebulizers effectively deliver asthma medications in a fine mist through masks sized differently to fit infants through adults, or through T-tubes with mouthpieces. Their use tends to be particularly easy, requiring only usual inspiration and expiration through the connection to the nebulizer. Nebulized asthma treatments are especially useful for infants, young children and some elderly patients who are unable to use an MDI. Use of a nebulizer can be more time-consuming.
Dr. Bray will prescribe the inhaled medication that is most appropriate for you. If you have any questions about your prescribed inhaled medications or their proper use. make sure to contact Dr. Bray. Many inhaled asthma medications are intended to be used on a daily basis to keep your airways open, even when you are not experiencing symptoms. It is important to follow Dr. Bray's instructions to ensure that you are optimally managing your asthma.
When you should see an asthma specialist:
Dr. Bray & his staff can provide information to assist Permian Basin asthma patients in determining when they may need a consultation or ongoing specialty care. Patients should schedule a visit if they:
Asthma is not curable but it can also always be very well controlled with proper and good education, proper medication and allergy therapy if indicated. A personalized. Workable effective program can be accomplished when the asthma expert and the patient work together as a team. Consistency and compliance with your asthma plan will pay off with much better health.
If you suffer from asthma, you are all too familiar with the symptoms. Allergies start to flare
and then it begins: coughing, wheezing, chest tightness, shortness of breath, inflammation in
the breathing tubes, and excess mucus in the airways. You are also likely to be familiar with the
accepted traditional treatments of asthma consisting of a daily regimen of one or more of these
types of medications: corticosteroid inhalers, breathing treatments with albuterol and
budesonide, antihistamines and montelukast. Some patients require a prednisone burst, or in
severe asthma, daily prednisone for several weeks. A few patients' asthma may become so
severe that they are forced to stay on prednisone for many months to many years with all the
'as}ociated side effects. For most people, basic medications are sufficient to produce good
relief and long-term excellent improvement. However, some asthma is simply more difficult to
treat. Why?
Asthma that is very difficult to treat may be caused by a variety of different things. Likely possible issues may include one or more of the following: patient non-compliance, when the patient doesn't consistently take their medication as directed by the physician, a type of immunoglobulin called !g£, or special white blood cells called eosinophils. Let's examine each of these individually.
First, non-compliance is often a very common issue that is at the root of many poor medical outcomes. A patient with a severe asthma has absolutely no hope of staying well if he or she will not follow the directives of their physician. Always remember, the physician's goal of treatment is the healing or improvement of the medical condition of his or her patient. The patient and physician must form a cooperative working team, with good communication both ways.
Second, excess lgE, an antibody produced by the body, activates mast cells in response to allergic triggers. If produced in increased quantities, lgE results in the release of large amounts
of histamine and other allergic mediators which in turn, cause inflammation, swelling and
airway tightness characteristic of active asthma. This type of asthma is termed allergic asthma.
Third, eosinophils, normally present in very small amounts in the blood are helpful in fighting
off some diseases. If the numbers of eosinophils increase in the tissues lining the airways, it can
result in eosinophilic asthma resistant to typical therapy. In all three of these situations, happily,
there are new types of treatment that can be utilized along with more traditional therapy to
control difficult asthma. This new type of therapy developed for eosinophilic asthma and
allergic asthma are in a new group of medications known as biologics.
Biologics are often given as complementary medications, meaning they are given in addition to your regular preventative medications. There are multiple benefits to adding a biologic to a severe asthmatic's treatment plan, the most important of which is a proven reduction in exacerbations and hospitalizations from uncontrolled asthma. Also worthy of note is the convenience factor of the dosing schedule as biologics are dosed on a bi-weekly, monthly or bi-monthly schedule depending on the medication. Finally, the importance of a reduction or the complete removal of oral steroids from a patient's asthma treatment is a great benefit. The less we have to prescribe these types of steroids to a patient, the better it is for the patient.
Fasenra, Nucala, and Xo/air are three of the major biologics. Both Fasenra and Nucala are for eosinophilic asthma only and are limited to ages 12 and over. Fasenra works by targeting and eliminating excessive eosinophils from the body within 24 hours, thereby reducing the amount of asthma-related chemical mediators and lessening the chances for an asthma flare. It is dosed every 8 weeks after the first 2 months. Nucala works by targeting and disabling a chemical called lnterleukin-5 that activates eosinophils. Fewer activated eosinophils means less mediator release causing increased asthma. It is a once monthly injection and builds up over time in the body. Xolair is the only biologic for allergic asthma and chronic hives. It blocks lgE, the chemical that causes the release of potent chemical mediators involved in causing asthma. It is an injection given every 2 or 4 weeks and is approved for ages 6 and over.
Although biologics are not right for all circumstances, they have made a major difference in the lives of our patients with eosinophilic asthma, severe allergic asthma, or even chronic hives uncontrolled by conventional means. Since these medicines are given infrequently, they are also helpful in patients who have had a difficult time taking multiple daily medications longterm. Unfortunately, although effective, these drugs are very expensive and insurance companies can be resistant to approving them for payment. If you are interested in or have questions about whether or not biologics are right for you, please contact our office and set up an appointment for a consultation with Dr. Bray.